Network Slicing is a new network architecture, which will enable network operators to provide dedicated virtual networks to specific vertical customers over the 5G network infrastructure. Using Network Slicing, 5G networks offer significantly faster connections and lower latency which facilitates new use cases such as the eHealth video streaming for emergency response teams.
As part of the H2020 €8 million EU funded SliceNet project (https://slicenet.eu/), a number of partners including Cork Institute of Technology, with MEC-based ML/AI applications for 5G test-bed deployments, and RedZinc with its wearable video streaming are developing AI and video streaming applications for emergency response. CIT has designed a MEC-based TeleStroke Assessment service, which can be accessed on demand by paramedics in the ambulance, to assess symptoms of patients suspected of suffering from a stroke. RedZinc has developed and launched a wearable video camera using Augmented Reality features, with an accompanying managed network service, for paramedics to communicate back to hospitals and get expert medical advice for their remote patients.
A key aim in the SliceNet project is to demonstrate a verticals-oriented 5G network, focused on control of end-to-end Network Sliced services. Dedicated ‘slices’ of the network are guaranteed, to ensure the quality of service (QoS) necessary for the delivery of mission critical services, such as emergency telemedicine. In 2019, SliceNet partners will coordinate a smart health use case that prototypes ML/AI applications at the 5G network edge (MEC) for prehospital in-ambulance diagnostics.
Stroke is a leading cause of death and disability worldwide. In Ireland, approximately 10,000 people have a stroke related event annually, with 7,000 acute hospital admissions and upwards of 30,000 people living in the community with disabilities as a result of stroke. The direct cost to the State is up to €557 million a year.
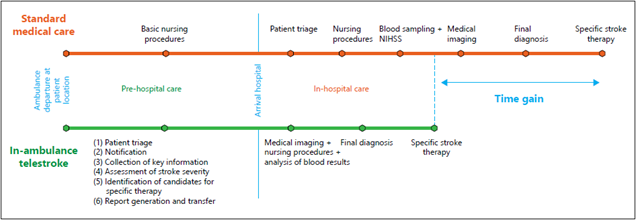
In recent years significant progress has been made through in-hospital stroke management, but a scalable solution to optimize prehospital in-ambulance care has not yet been established. Solving this problem could speed up treatment initiation by early activation of the in-hospital stroke response, thereby curtailing the risk of misdiagnosis, reducing the proportion of missed opportunities for treatment with intravenous thrombolysis and/or endovascular treatment, and avoiding patient admission to inadequate clinical facilities[1].
[1] Development and Pilot Testing of 24/7 In-Ambulance Telemedicine for Acute Stroke
